Fibromyalgia is a complex condition that involves heightened sensitivity to pain. Stimuli that would normally be painless, such as being touched, may be painful to someone suffering from fibromyalgia. The exact causes are not clear and almost certainly vary across populations. However, it appears that genetic factors, along with triggering events like infections or physical or emotional traumas, can lead to the development of fibromyalgia. Damaged nerves lose the ability to properly regulate pain signaling, and there are abnormal increases in pain-signaling chemicals in the brain. Phytocannabinoids like tetrahydrocannabinol (THC) and cannabidiol (CBD) possess neuroprotective properties which may make them suitable for treating fibromyalgia. As a review article on cannabinoids and neuroprotection stated, cannabinoids can help protect cells at least partially through prevention of excitotoxicity, along with antioxidant and anti-inflammatory effects.
Several human studies have examined the impact of THC and CBD on symptoms of fibromyalgia. A 2006 study conducted at a German university reported that between 2.5 – 15mg of isolated THC reduced the pain of fibromyalgia patients. However, five of the nine patients withdrew due to adverse side effects of THC, which is not surprising given that isolated THC is commonly reported to cause more discomfort than whole-plant formulations.
A more extensive study published in October 2020 by Brazilian researchers used a double-blind, placebo-controlled methodology to examine the impact of a whole-plant, THC-rich infused oil (24.44mg/mL THC and 0.51mg/mL CBD) on fibromyalgia symptoms among 17 women (eight in the cannabis group, nine in the placebo group). The initial dose was only 1.22mg THC per day, which was increased as needed by each participant. The average dose after patients were evaluated was only 4.4mg THC, which while relatively low was still reported to be effective. Symptoms were measured through the Fibromyalgia Impact Questionnaire (FIQ), in which higher scores reflect more severe symptoms. The THC group experienced a reduction in score from 75.5 to 30.5, whereas the placebo group only went from 70.2 to 61.2. Areas of particular improvement were the “feel good”, “pain”, and “fatigue” items. Researchers concluded, “Phytocannabinoids can be a low-cost and well-tolerated therapy to reduce symptoms and increase the quality of life of patients with fibromyalgia.”
The most recent study to examine medical cannabis for fibromyalgia symptoms was published in 2021 in the Journal of Cannabis Research. Five types of cannabis were used, two of which had similar THC and CBD contents, while three were predominantly THC with little CBD. Interestingly, one of the administration methods essentially involved making a tea by boiling minced cannabis in water and milk (referred to as the decoction). Other methods of administration included vaporization or sublingual administration with an olive oil extract.
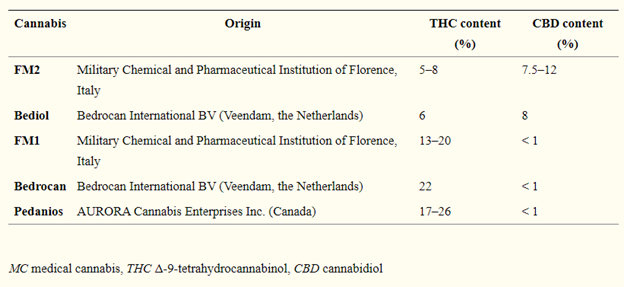
38 patients, 36 women and 2 men, were followed in the study, although due to various issues only 30 patients completed at least one month of therapy. Several of these patients, and those who had dropped out, experienced side effects like confusion, dry mouth, and vomiting, which may have been related to the use of THC-dominant and balanced (referred to as hybrid) THC and CBD cultivars. The patients included were deemed resistant to other conventional treatment drugs, so their situations may have been more complicated overall than fibromyalgia patients who do respond to conventional drugs. For many patients, starting out with CBD-dominant cannabis cultivars is necessary to avoid side effects, but such options were not explored in this study.
All patients started with the decoction; six patients who responded switched to either vaporization or the olive oil extract due to unpleasant taste. Three patients also ended up switching from the hybrid cultivars to a THC dominant cultivar for enhanced pain relief, suggesting that THC was more effective for some patients than CBD. Daily doses were reported for patients who complete at least three months of therapy. Patients who used the THC-dominant cultivars in decoction form ingested an average of 55.2mg THC per day, while those who used oil extracts ingested an average of 17.5mg THC per day. Patients who used the hybrid THC and CBD cultivars in decoction form ingested an average of 23.4mg THC and 34.7mg CBD per day, while those who used oil extracts ingested an average of 2.4mg THC and 2mg CBD per day. It is unclear why the doses used from the oil were so much smaller than the decoction, and the researchers stated that the small sample size and potential bias warrant cautious interpretation of the results.
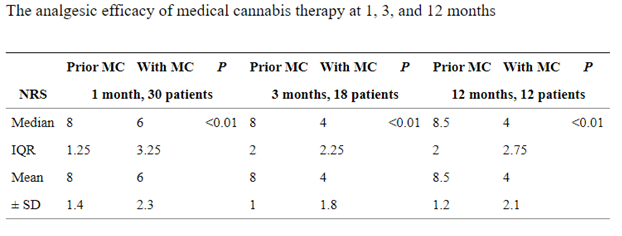
Despite side effects, on average, there were positive effects from the medical cannabis treatments. For 20 of the 30 patients, the therapy was associated with reduced pain intensity of at least 30% at the 1-month follow-up; for those who continued in the study, this average reduction persisted at 3 months and 12 months. Five patients experienced between 30-50% decrease in intensity, while 12 reported even greater relief of more than 50% decrease in intensity. The chart below summarizes pain reduction scores for each period analyzed. Importantly, no tolerance effect was observed, showing that patients could maintain benefits without needing to increase their doses over time, even after 12 months.
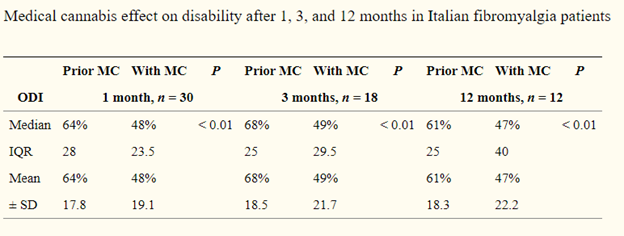
Another chart showed an improvement in a disability index, indicating improved function overall.
Patients with fibromyalgia often need to rely on multiple classes of drugs to maintain a reasonable quality-of-life. 50% of responsive patients were able to discontinue other medications by using medical cannabis. Drugs that were reduced include acetaminophen, opioids, nerve pain drugs like pregabalin (Lyrica), and benzodiazepines.
Overall, this study was quite complex due to the numerous types of cannabis used, the various administration methods, and the differing amounts of time that different patients used medical cannabis therapy. More research is needed, but this study and others do support the potential efficacy of THC and CBD in reducing pain and improving quality-of-life overall. Further studies should examine the impact of different cultivars of THC-rich cannabis and the effects of higher doses of CBD delivered with CBD-dominant cultivars. Studies examining the impact of other nonpsychotropic cannabinoids like THCA, CBDA, and CBG are also warranted, since there is a lower probability of adverse effects with those compounds, but their neuroprotective and anti-inflammatory properties may still confer significant benefits.
